- Services
Technology Capabilities
Technology Capabilities- Product Strategy & Experience DesignDefine software-driven value chains, create purposeful interactions, and develop new segments and offerings
- Digital Business TransformationAdvance your digital transformation journey.
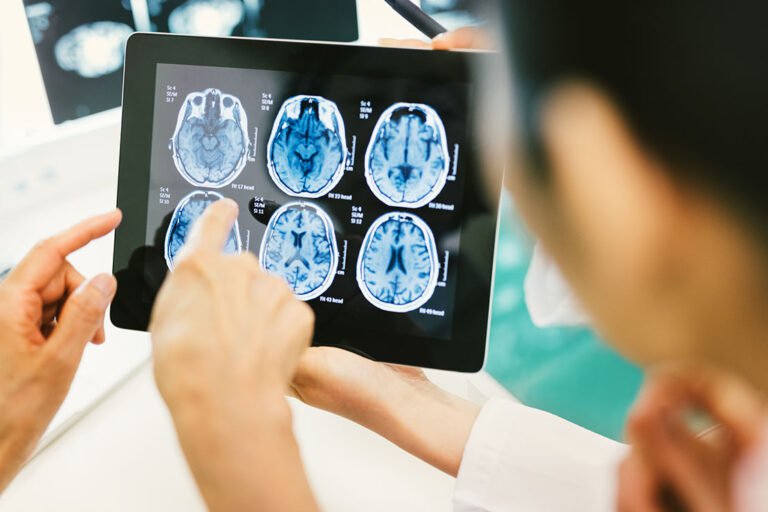
- Intelligence EngineeringLeverage data and AI to transform products, operations, and outcomes.
- Software Product EngineeringCreate high-value products faster with AI-powered and human-driven engineering.
- Technology ModernizationTackle technology modernization with approaches that reduce risk and maximize impact.
- Embedded Engineering & IT/OT TransformationDevelop embedded software and hardware. Build IoT and IT/OT solutions.
- Industries
- GlobalLogic VelocityAI
- Insights
BlogsGlobalLogicJuly 27, 2023Exploring Snowpark and Streamlit for Data Science
I’m Janki Makwana, a Data Scientist at GlobalLogic. I have been working with a major re...
 BlogsJuly 18, 2023Manik Jandial
BlogsJuly 18, 2023Manik JandialView on payment industry modernisation: Enablers of change
Welcome to the second part of our two-part series on the evolving payment industry! In ...

- About
BlogsBlogsBlogsBlogsBlogsBlogsBlogsBlogsBlogsBlogs